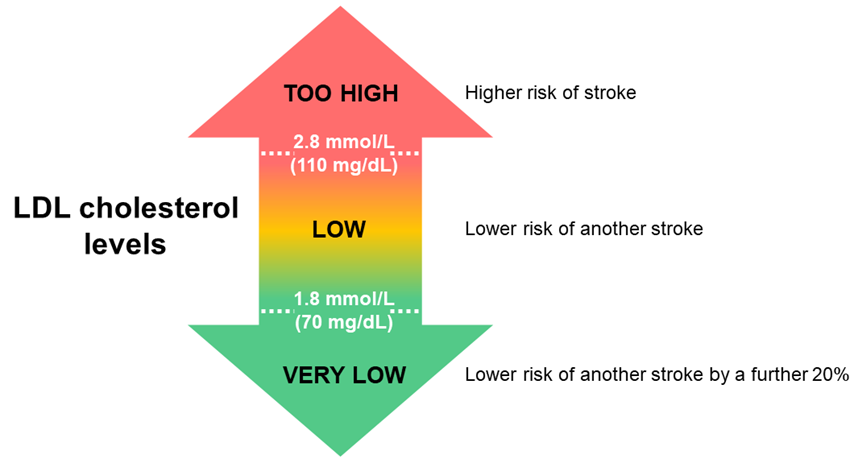
National Stroke Guidelines strongly recommend taking medication to lower LDL cholesterol to under 1.8 mmol/L (70 mg/dL).
- Recommended for patients after stroke caused by a blood clot.
- Helps to prevent another stroke and/or heart attack.
What’s important to know?
Cholesterol is a type of fat in the body. A cholesterol test usually shows your total cholesterol levels. This includes LDL (low-density lipoprotein), HDL (high-density lipoprotein), and triglycerides.
LDL cholesterol is “bad” cholesterol. It can build up inside arteries and block the flow of blood. It can also lead to blood clots. Blocked arteries and blood clots can cause stroke and heart disease.
HDL cholesterol is “good” cholesterol. It protects against stroke and heart disease.
- About half of all adults in Australia have high LDL cholesterol (above 5 mmol/L, 190 mg/dL).
- About 40% of people who have had a stroke will have another in the next 10 years. Lowering LDL cholesterol can lower the risk of another stroke.
- Healthy lifestyle changes are important for lowering LDL cholesterol. These include a healthy diet, physical activity, not smoking, and drinking less alcohol. Even after healthy lifestyle changes, medication is often needed to lower LDL cholesterol to the target level.
- Statins are the most commonly used type of medication to lower LDL cholesterol. Additional medication on top of statins may be needed to lower LDL cholesterol to the target level. Even if medication is used, healthy lifestyle changes are important.
- Side effects from lowering LDL cholesterol are rare. After lowering LDL cholesterol, 1% of people may be at risk of intracerebral haemorrhage, and 6–7% of people may be at risk of diabetes.
- The benefits of preventing another stroke and/or heart attack outweigh the rare risks.
What’s the research behind this recommendation?
There is moderately strong research behind this recommendation.
One study (Amarenco et al. 2020) compared the effects of lowering LDL cholesterol to a low level (2.3–2.8 mmol/L, 90–110 mg/dL) versus a very low level (under 1.8 mmol/L, 90 mg/dL). It showed that a very low level of LDL cholesterol is better for preventing another stroke. Over 3½ years, another stroke or heart attack occurred in 1 in 9 patients with low LDL cholesterol, versus 1 in 11 patients with very low LDL cholesterol. In this study, a third of patients needed additional medication on top of statins to lower LDL cholesterol to a very low level.
Another study (Baigent et al. 2010) looked at the combined results of 26 studies with 170,000 patients in total. There was a clear link between lowering LDL cholesterol and lowering the risk of stroke. On average, lowering LDL cholesterol by 1 mmol/L (38 mg/dL) lowered the risk of stroke by 20%.
Additional information
- Any medication and potential side effects should be discussed with a doctor.
- Examples of high dose statins are atorvastatin 80 mg and rosuvastatin 40 mg.
- If LDL cannot be lowered to the target level using statins, ezetimibe on top of statins should be trialed. For example, an extra 10 mg ezetimibe every day.
- If LDL cannot be lowered to the target level using ezetimibe on top of statins, a PCSK9 inhibitor medication should be trialed. For example, an extra 140 mg evolocumab every two weeks.
- High dose statins may cause side effects. If this occurs, ezetimibe on top of lower dose statins should be trialled. Medication should be trialed to lower LDL to a level that is low but with fewer side effects.
- Treatment to lower cholesterol is tracked in the National Stroke Audit and included in the Acute Stroke Clinical Care Standard. It is stated as a combined treatment approached together with treatment to lower blood pressure and antithrombotic medication (blood thinning medication).
Questions to ask your doctor
- What are my cholesterol levels?
- What do my cholesterol levels mean?
- Do I need medication to lower my cholesterol?
- Which medication is right for me?
- What are the potential side effects?
- How long will I need to take medication?
- How else can I lower my risk of another stroke?
- How often should I have my cholesterol levels checked?
Learn more
- Cholesterol (Better Health Channel)
- Preventing stroke
- Medication after stroke
About this recommendation
Stroke Foundation's guidelines provide recommendations for managing stroke according to the latest research. Being informed helps to ensure the best care and outcomes. This resource was co-designed with consumers to provide accessible and useful information for stroke survivors and carers. The information in this resource has been adapted from the Clinical Guidelines for Stroke Management.
For more help
- Talk to your doctor (GP or specialist)
- Call StrokeLine 1800 787 653
- Visit Stroke Foundation website
- Find Stroke Foundation on Facebook
- Find Stroke Foundation on Twitter and Instagram
- Connect with others on EnableMe
- Connect with others on Young Stroke Project
